In an age of digital healthcare and the seamless exchange of sensitive patient information, it’s crucial for healthcare providers and organizations to prioritize the security and privacy of patient data.
What is HIPAA?
The Health Insurance Portability and Accountability Act (HIPAA) is a set of federal regulations that enforces the protection of patients’ medical records and personal health information (PHI).
HIPAA compliance extends to all entities that handle PHI, and this includes secure file sharing practices.
The Importance of Secure File Sharing in Healthcare
Secure file sharing is an integral part of modern healthcare operations. Healthcare professionals need to share patient records, test results, and other sensitive information swiftly and efficiently, often across various departments and healthcare facilities. The challenge lies in maintaining the privacy and security of this data.
Failure to secure patient data during file sharing can have severe consequences. Data breaches can lead to unauthorized access to medical records, identity theft, and financial fraud, all of which can severely harm patients and damage an organization’s reputation. Moreover, non-compliance with HIPAA can result in hefty fines and legal penalties.
Understanding HIPAA Compliance
HIPAA was enacted in 1996 with the primary aim of protecting patient privacy and ensuring the security of electronic health records. It consists of several rules which outline the requirements for safeguarding PHI.
- The Privacy Rule
- The Security Rule
- The Breach Notification Rule
The Privacy Rule mandates that healthcare providers and related organizations must establish protocols for protecting patient information. The Security Rule, on the other hand, focuses on the technical and physical safeguards that should be in place to secure PHI.
The Breach Notification Rule requires the timely notification of patients, the U.S. Department of Health and Human Services (HHS), and, in some cases, the media when a data breach occurs.
What Happens if You Violate HIPAA?
HIPAA penalties vary based on the severity of the violation. The Office for Civil Rights (OCR) is the agency within the U.S. Department of Health and Human Services that investigates complaints about failures to protect the privacy or security of health information.
OCR prefers to resolve HIPAA violations using non-punitive measures, such as voluntary compliance or issuing technical guidance to help covered entities address areas of non-compliance. However, if the violations are serious, have been allowed to persist for a long time, or if there are multiple areas of noncompliance, financial penalties may be appropriate.
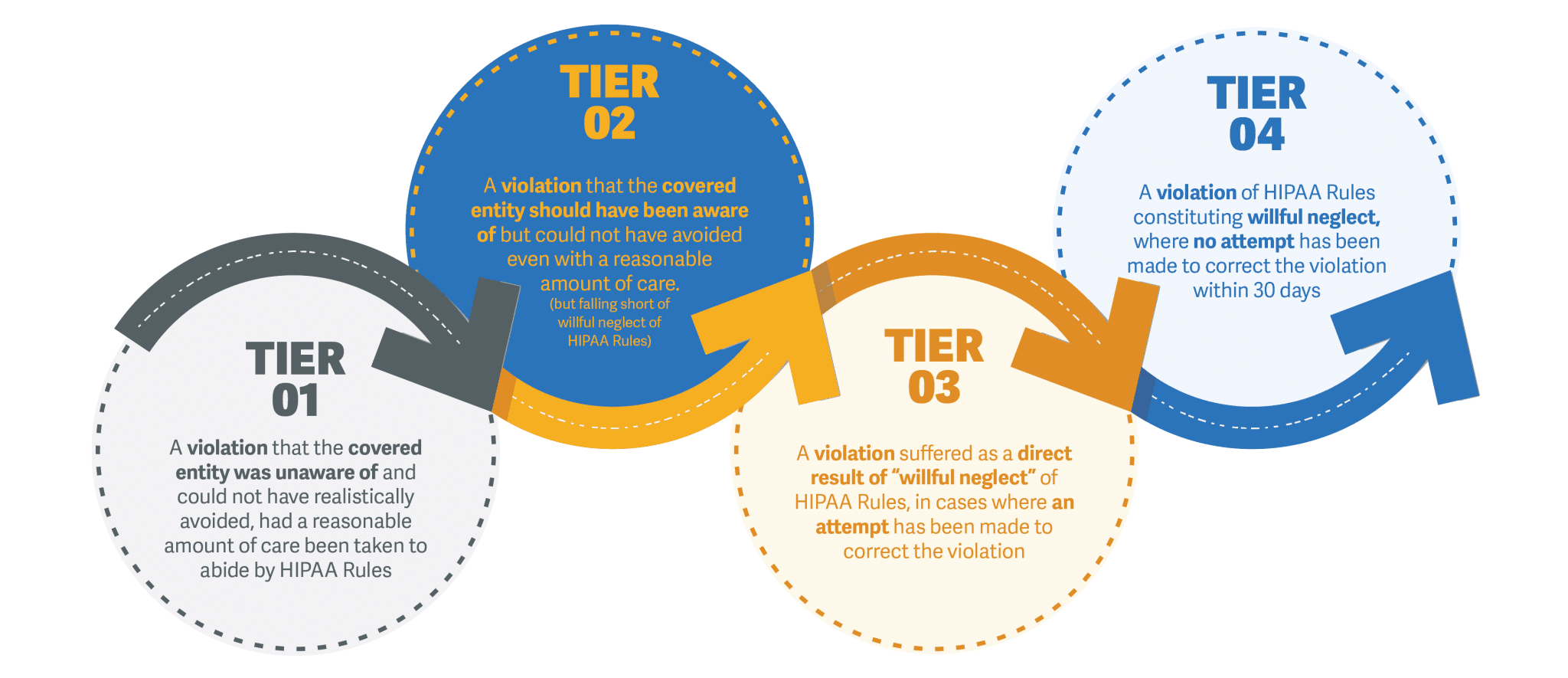
The four categories used for the penalty structure are as follows:
- Tier 1: A violation that the covered entity was unaware of and could not have realistically avoided, had a reasonable amount of care been taken to abide by HIPAA Rules
- Tier 2: A violation that the covered entity should have been aware of but could not have avoided even with a reasonable amount of care. (but falling short of willful neglect of HIPAA Rules)
- Tier 3: A violation suffered as a direct result of “willful neglect” of HIPAA Rules, in cases where an attempt has been made to correct the violation
- Tier 4: A violation of HIPAA Rules constituting willful neglect, where no attempt has been made to correct the violation within 30 days
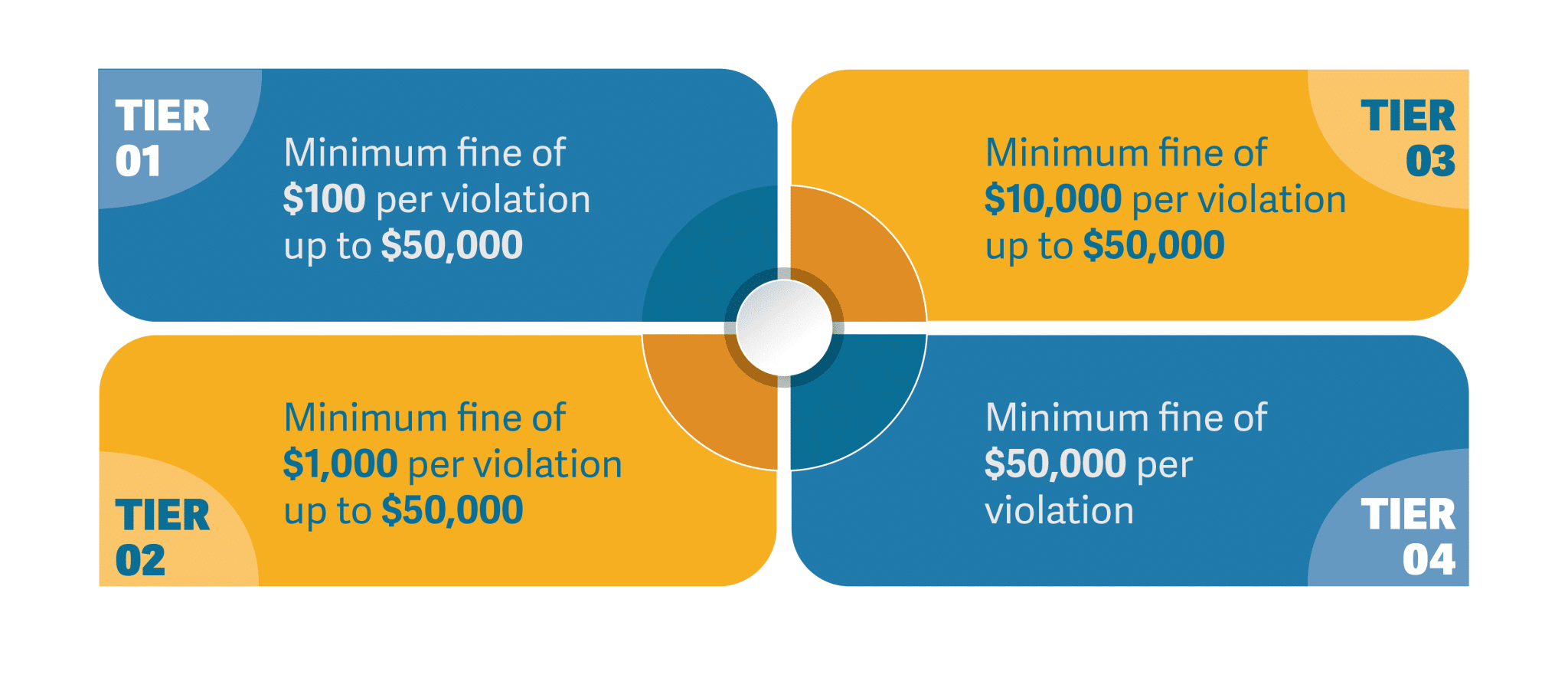
Each category of violation carries a separate HIPAA penalty. It’s up to OCR to determine a financial penalty within the appropriate range. OCR considers a number of factors when determining penalties, such as the length of time a violation was allowed to persist, the number of people affected, and the nature of the data exposed.
An organization’s willingness to assist with an OCR investigation is also taken into account. The general factors that can affect the amount of the financial penalty also include prior history, the organization’s financial condition, and the level of harm caused by the violation.
- Tier 1: Minimum fine of $100 per violation up to $50,000
- Tier 2: Minimum fine of $1,000 per violation up to $50,000
- Tier 3: Minimum fine of $10,000 per violation up to $50,000
- Tier 4: Minimum fine of $50,000 per violation
Best Practices for Secure File Sharing in HIPAA Compliance
Encryption
Utilize end-to-end encryption to protect the confidentiality and integrity of patient data during transmission and storage. Encryption ensures that even if unauthorized individuals gain access to the data, they cannot decipher it without the appropriate decryption key.
Access Control
Implement strict access controls to limit the people who can view or edit sensitive patient data. Use role-based access to ensure that only authorized personnel can access particular files.
Audit Trails
Maintain audit trails to track who accessed and modified patient records. This helps in identifying any suspicious activity and maintaining accountability.
Secure Platforms
Choose file-sharing platforms and solutions that are HIPAA-compliant and offer robust security features. These platforms should provide features like data loss prevention, automatic logoff, and secure authentication.
Employee Training
Ensure that all staff members are trained on HIPAA regulations and secure file sharing best practices. Regular training and awareness programs can help prevent unintentional violations.
Regular Audits
Conduct regular internal audits to identify vulnerabilities and potential areas of non-compliance. Address any issues promptly to maintain the highest level of data security.
Business Associate Agreements (BAAs)
If you work with third-party vendors, such as cloud storage providers, make sure to have BAAs in place. These agreements stipulate the responsibilities and obligations of these vendors in protecting patient data.
Mobile Device Management
If healthcare professionals use mobile devices for file sharing, implement mobile device management (MDM) solutions to secure these devices and the data they contain.
The consequences of non-compliance with HIPAA are significant, ranging from fines to damage to an organization’s reputation. Therefore, it is crucial for healthcare providers and organizations to prioritize secure file sharing practices that are in line with HIPAA regulations.
Protecting the privacy and security of patient data is not only a legal obligation but also an ethical responsibility in the healthcare industry.
ShareVault virtual data rooms are used by healthcare organizations worldwide. It’s a data room solution equipped with the industry’s most advanced document-sharing capabilities and highly granular access control policies.
Using ShareVault, health organizations can confidently share sensitive patient information and company data with payers, providers, patient care teams, and relevant stakeholders without compromising information security.